Abstract
Research Article
Partial SHOX duplications associated with various cases of congenital uterovaginal aplasia (MRKH syndrome): A tangible evidence but a puzzling mechanism
Daniel Guerrier* and Karine Morcel
Published: 24 March, 2021 | Volume 4 - Issue 1 | Pages: 001-008
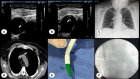
The Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome is the most severe form of congenital malformation of the inner female reproductive tract. It is diagnosed as such when the uterus, the upper vagina and optionally the Fallopian tubes are absent. It accounts for approximately 1 in 5000 live-born females and has been classified in two subtypes: type 1 in the presence of isolated uterovaginal aplasia and type 2 when associated in various combinations with extragenital malformations of the kidneys, skeleton, heart and auditory system. Most cases of MRKH syndrome are sporadic, although a significant number of many familial cases have been reported to date. Despite numerous studies, the genetics of the syndrome remains largely unknown and appears to be heterogeneous: chromosomal abnormalities and some candidate gene variants appear to be associated with a few cases; others have been suggested but not yet confirmed. To date, mainly the GREB1L gene appears to be a serious candidate. Among the remaining hypotheses, the controversial contribution of partial duplications of the SHOX gene is still puzzling, as the deficiency of this gene is a major cause of skeletal adysplasia syndromes. We have attempted to resolve this controversy in a study of 60 MRKH cases. Our results tend to show that SHOX duplications can be the origin of a genetic mechanism responsible for MRKH syndrome.
Read Full Article HTML DOI: 10.29328/journal.jgmgt.1001006 Cite this Article Read Full Article PDF
Keywords:
CNV; Congenital uterovaginal aplasia; Duplication; MRKH syndrome; SHOX
References
- Morcel K, Camborieux L, Guerrier D. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Orphanet J Rare Dis. 2007; 14: 13. https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-2-13
- Jacquinet A, Millar D, Lehman A. Etiologies of uterine malformations. Am J Med Genet A. 2016; 170: 2141-2172. https://onlinelibrary.wiley.com/doi/abs/10.1002/ajmg.a.37775
- Herlin M, Bjørn AM, Rasmussen M, et al. Prevalence and patient characteristics of Mayer-Rokitansky-Küster-Hauser syndrome: a nationwide registry-based study. Hum Reprod. 2016; 31: 2384-2390. https://academic.oup.com/humrep/article/31/10/2384/2198191
- Acién P, Acién M, Sánchez-Ferrer M. Complex malformations of the female genital tract. New types and revision of classification. Hum Reprod. 2004; 19: 2377-2384. https://academic.oup.com/humrep/article/19/10/2377/589016
- Oppelt P, Renner SP, Brucker S, et al. The VCUAM (Vagina Cervix Uterus Adnex-associated Malformation) classification: a new classification for genital malformations. Fertil Steril. 2005; 84: 1493-1467. https://www.fertstert.org/article/S0015-0282(05)02786-X/fulltext
- Acién P, Acién MI. The history of female genital tract malformation classifications and proposal of an updated system. Hum Reprod Update. 2011; 17: 693-705. https://academic.oup.com/humupd/article/17/5/693/759275
- Grimbizis GF, Gordts S, Di Spiezio Sardo A, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. 2013; 28: 2032-2044. https://academic.oup.com/humrep/article/28/8/2032/658933
- Biason-Lauber A, Konrad D. WNT4 and sex development. Sex Dev. 2008; 2: 210-218. https://www.karger.com/Article/Abstract/152037
- Fontana L, Gentilin B, Fedele L, et al. Genetics of Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Clin Genet. 2017; 91: 233-246. https://onlinelibrary.wiley.com/doi/full/10.1111/cge.12883
- Deng S, He Y, Chen N, et al. Spectrum of Type I and Type II Syndromes and Associated Malformations in Chinese Patients with Mayer-Rokitansky-Küster-Hauser Syndrome: A Retrospective Analysis of 274 Cases. J Pediatr Adolesc Gynecol. 2019; 32: 284-287. https://www.jpagonline.org/article/S1083-3188(18)30260-2/fulltext
- Herlin MK, Petersen MB, Brännström M. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome: a comprehensive update. Orphanet J Rare Dis. 2020; 15: 214. https://ojrd.biomedcentral.com/articles/10.1186/s13023-020-01491-9
- Petrozza JC. Mayer-Rokitansky-Küster-Hauser syndrome and associated malformations: are they as common as we think? Fertil Steril. 2016; 106: 1047-1048. https://www.fertstert.org/article/S0015-0282(16)61388-2/fulltext
- Griffin JE, Edwards C, Madden JD, et al. Congenital absence of the vagina. The Mayer-Rokitansky-Kuster-Hauser syndrome. Ann Intern Med. 1976; 85: 224-236. https://www.acpjournals.org/doi/10.7326/0003-4819-85-2-224
- Opitz JM. Vaginal atresia (von Mayer-Rokitansky-Küster or MRK anomaly) in hereditary renal adysplasia (HRA). Am J Med Genet. 1987; 26: 873-876. https://onlinelibrary.wiley.com/doi/abs/10.1002/ajmg.1320260414
- Guerrier D, Mouchel T, Pasquier L, et al. The Mayer-Rokitansky-Küster-Hauser syndrome (congenital absence of uterus and vagina)--phenotypic manifestations and genetic approaches. J Negat Results Biomed. 2006; 5: 1. https://jnrbm.biomedcentral.com/articles/10.1186/1477-5751-5-1
- Schouten JP, McElgunn CJ, Waaijer R, et al. Relative quantification of 40 nucleic acid sequences by multiplex ligation-dependent probe amplification. Nucleic Acids Res. 2002; 30: e57. https://academic.oup.com/nar/article/30/12/e57/2380384
- Bernardini L, Gimelli S, Gervasini C, et al. Recurrent microdeletion at 17q12 as a cause of Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome: two case reports. Orphanet J Rare Dis. 2009; 4: 25. https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-4-25
- Nik-Zainal S, Strick R, Storer M, et al. High incidence of recurrent copy number variants in patients with isolated and syndromic Müllerian aplasia. J Med Genet. 2011; 48: 197-204. https://jmg.bmj.com/content/48/3/197
- Ledig S, Schippert C, Strick R, et al. Recurrent aberrations identified by array-CGH in patients with Mayer-Rokitansky-Küster-Hauser syndrome. Fertil Steril. 2011; 95: 1589-1594. https://www.fertstert.org/article/S0015-0282(10)02168-0/fulltext
- Xia M, Zhao H, Qin Y, et al. LHX1 mutation screening in 96 patients with müllerian duct abnormalities. Fertil Steril. 2012; 97: 682-685. https://www.fertstert.org/article/S0015-0282(11)02857-3/fulltext
- Ledig S, Brucker S, Barresi G, et al. Frame shift mutation of LHX1 is associated with Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome. Hum Reprod. 2012; 27: 2872-2875. https://academic.oup.com/humrep/article/27/9/2872/625703
- Sandbacka M, Laivuori H, Freitas E, et al. TBX6, LHX1 and copy number variations in the complex genetics of Müllerian aplasia. Orphanet J Rare Dis. 2013; 8: 125. https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-8-125
- Williams LS, Demir Eksi D, Shen Y, et al. Genetic analysis of Mayer-Rokitansky-Kuster-Hauser syndrome in a large cohort of families. Fertil Steril. 2017; 108: 145-151. https://www.fertstert.org/article/S0015-0282(17)30398-9/fulltext
- Tewes A-C, Rall KK, Römer T, et al. Variations in RBM8A and TBX6 are associated with disorders of the müllerian ducts. Fertil Steril. 2015; 103: 1313-1318. https://www.fertstert.org/article/S0015-0282(15)00136-3/fulltext
- Pan HX, Luo GN, Wan SQ, et al. Detection of de novo genetic variants in Mayer-Rokitansky-Küster-Hauser syndrome by whole genome sequencing. Eur J Obstet Gynecol Reprod Biol X. 2019; 4: 100089. https://www.sciencedirect.com/science/article/pii/S259016131930122X?via%3Dihub
- Herlin MK, Le VQ, Allan T Højland AT, Ernst A, Okkels H, et al. Whole-exome sequencing identifies a GREB1L variant in a three-generation family with Müllerian and renal agenesis: a novel candidate gene in Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. A case report. Hum Reprod. 2019; 34: 1838-1846. PubMed: https://pubmed.ncbi.nlm.nih.gov/31424080/
- Jacquinet A, Boujemla B, Fasquelle C, et al. GREB1L variants in familial and sporadic hereditary urogenital adysplasia and Mayer-Rokitansky-Kuster-Hauser syndrome. Clin Genet. 2020; 98: 126-137. https://onlinelibrary.wiley.com/doi/abs/10.1111/cge.13769
- Brophy PD, Rasmussen M, Parida M, et al. A Gene Implicated in Activation of Retinoic Acid Receptor Targets Is a Novel Renal Agenesis Gene in Humans. Genetics. 2017; 207: 215-228. https://academic.oup.com/genetics/article/207/1/215/5930718
- Nakajima T, Sato T, Iguchi T, et al. Retinoic acid signaling determines the fate of the uterus from the mouse Müllerian duct. Reprod Toxicol. 2019; 86: 56-61. https://www.sciencedirect.com/science/article/pii/S0890623818306105?via%3Dihub
- Gervasini C, Grati R, Lalatta F, et al. SHOX duplications found in some cases with type I Mayer-Rokitansky-Kuster-Hauser syndrome. Genet Med. 2010; 12: 634-640. https://www.nature.com/articles/gim2010106
- Sandbacka M, Halttunen M, Jokimaa V, et al. Evaluation of SHOX copy number variations in patients with Müllerian aplasia. Orphanet J Rare Dis. 2011; 6: 53. https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-6-53
- Binder G. Short stature due to SHOX deficiency: genotype, phenotype, and therapy. Horm Res Paediatr. 2011; 75: 81-89. https://www.karger.com/Article/FullText/324105
- Bunyan DJ, Baker KR, Harvey JF, et al. Diagnostic screening identifies a wide range of mutations involving the SHOX gene, including a common 47.5 kb deletion 160 kb downstream with a variable phenotypic effect. Am J Med Genet A. 2013; 161A: 1329-1338. https://onlinelibrary.wiley.com/doi/abs/10.1002/ajmg.a.35919
- Marchini A, Ogata T, Rappold GA. A Track Record on SHOX: From Basic Research to Complex Models and Therapy. Endocr Rev. 2016; 37: 417-448. https://academic.oup.com/edrv/article/37/4/417/2567101
- Dehainault C, Laugé A, Caux-Moncoutier V, et al. Multiplex PCR/liquid chromatography assay for detection of gene rearrangements: application to RB1 gene. Nucleic Acids Res. 2004; 32: e139. https://academic.oup.com/nar/article/32/18/e139/998831
- Bendavid C, Pasquier L, Watrin T, et al. Phenotypic variability of a 4q34-->qter inherited deletion: MRKH syndrome in the daughter, cardiac defect and Fallopian tube cancer in the mother. Eur J Med Genet. 2007; 50: 66-72. https://www.sciencedirect.com/science/article/pii/S1769721206000991?via%3Dihub
- Morcel K, Watrin T, Pasquier L, et al. Utero-vaginal aplasia (Mayer-Rokitansky-Küster-Hauser syndrome) associated with deletions in known DiGeorge or DiGeorge-like loci. Orphanet J Rare Dis. 2011; 6: 9. https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-6-9
- Pontecorvi P, Bernardini L, Capalbo A, et al. Protein-protein interaction network analysis applied to DNA copy number profiling suggests new perspectives on the aetiology of Mayer-Rokitansky-Küster-Hauser syndrome. Sci Rep. 2021; 11: 448. https://www.nature.com/articles/s41598-020-79827-5
- Chen J, Wildhardt G, Zhong Z, et al. Enhancer deletions of the SHOX gene as a frequent cause of short stature: the essential role of a 250 kb downstream regulatory domain. J Med Genet. 2009; 46: 834-839. https://jmg.bmj.com/content/46/12/834
- Benito-Sanz S, Barroso E, Heine-Suner D, et al. Clinical and molecular evaluation of SHOX/PAR1 duplications in Leri-Weill dyschondrosteosis (LWD) and idiopathic short stature (ISS). J Clin Endocrinol Metab. 2011; 96: E404-412. https://doi.org/10.1210/jc.2010-1689
- Rao E, Weiss B, Fukami M, et al. FISH-deletion mapping defines a 270-kb short stature critical interval in the pseudoautosomal region PAR1 on human sex chromosomes. Hum Genet. 1997; 100: 236-239. https://link.springer.com/article/10.1007/s004390050497
- Ogata T, Matsuo N, Nishimura G. SHOX haploinsufficiency and overdosage: impact of gonadal function status. J Med Genet. 2001; 38: 1-6. https://jmg.bmj.com/content/38/1/1
- Benito-Sanz S, Thomas NS, Huber C, et al. A novel class of Pseudoautosomal region 1 deletions downstream of SHOX is associated with Leri-Weill dyschondrosteosis. Am J Hum Genet. 2005; 77: 533-544. https://www.cell.com/ajhg/fulltext/S0002-9297(07)61002-7
- Benito-Sanz S, Belinchon-Martínez A, et al. Identification of 15 novel partial SHOX deletions and 13 partial duplications, and a review of the literature reveals intron 3 to be a hotspot region. J Hum Genet. 2017; 62: 229-234. https://www.nature.com/articles/jhg2016113
- Tiecke E, Bangs F, Blaschke R, et al. Expression of the short stature homeobox gene SHOX is restricted by proximal and distal signals in chick limb buds and affects the length of skeletal elements. Dev Biol. 2006; 298: 585-596. https://www.sciencedirect.com/science/article/pii/S0012160606009900?via%3Dihub
- Thomas NS, Harvey JF, Bunyan DJ, et al. Clinical and molecular characterization of duplications encompassing the human SHOX gene reveal a variable effect on stature. Am J Med Genet A. 2009; 149A: 1407-1414. https://onlinelibrary.wiley.com/doi/abs/10.1002/ajmg.a.32914
- Upners EN, Jensen RB, Rajpert-De Meyts E, et al. Short stature homeobox-containing gene duplications in 3.7% of girls with tall stature and normal karyotypes. Acta Paediatr. 2017; 106: 1651-1657. https://onlinelibrary.wiley.com/doi/abs/10.1111/apa.13969
- Ramirez JM, Rodríguez FA, Echeverría MI, et al. SHOX Duplication and Tall Stature in a Patient with Xq Deletion and Vascular Disease. Case Rep Genet. 2019; 2019: 2691820. https://www.hindawi.com/journals/crig/2019/2691820/
- Fukami M, Naiki Y, Muroya K, et al. Rare pseudoautosomal copy-number variations involving SHOX and/or its flanking regions in individuals with and without short stature. J Hum Genet. 2015; 60: 553-556. https://www.nature.com/articles/jhg201553
- Hirschfeldova K, Solc R. Comparison of SHOX and associated elements duplications distribution between patients (Lėri-Weill dyschondrosteosis/idiopathic short stature) and population sample. Gene. 2017; 627: 164-168. https://www.sciencedirect.com/science/article/pii/S0378111917304845?via%3Dihub
- Tropeano M, Howley D, Gazzellone MJ, et al. Microduplications at the pseudoautosomal SHOX locus in autism spectrum disorders and related neurodevelopmental conditions. J Med Genet. 2016; 53: 536-547. https://jmg.bmj.com/content/53/8/536
- Rall K, Eisenbeis S, Henninger V, et al. Typical and Atypical Associated Findings in a Group of 346 Patients with Mayer-Rokitansky-Kuester-Hauser Syndrome. J Pediatr Adolesc Gynecol. 2015; 28: 362-368. https://www.jpagonline.org/article/S1083-3188(14)00369-6/fulltext
- Kapczuk K, Iwaniec K, Friebe Z, et al. Congenital malformations and other comorbidities in 125 women with Mayer-Rokitansky-Küster-Hauser syndrome. Eur J Obstet Gynecol Reprod Biol. 2016; 207: 45-49. https://www.ejog.org/article/S0301-2115(16)30962-9/fulltext
- Rappold G, Blum WF, Shavrikova EP, et al. Genotypes and phenotypes in children with short stature: clinical indicators of SHOX haploinsufficiency. J Med Genet. 2007; 44: 306-313. https://jmg.bmj.com/content/44/5/306
- Turner DJ, Miretti M, Rajan D, et al. Germline rates of de novo meiotic deletions and duplications causing several genomic disorders. Nat Genet. 2008; 40: 90-95. https://www.nature.com/articles/ng.2007.40
- May CA, Shone AC, Kalaydjieva L, et al. Crossover clustering and rapid decay of linkage disequilibrium in the Xp/Yp pseudoautosomal gene SHOX. Nat Genet. 2002; 31: 272-275. https://www.nature.com/articles/ng918z
- Lien S, Szyda J, Schechinger B, et al. Evidence for heterogeneity in recombination in the human pseudoautosomal region: high resolution analysis by sperm typing and radiation-hybrid mapping. Am J Hum Genet. 2000; 66: 557-566. https://www.cell.com/ajhg/fulltext/S0002-9297(07)63430-2
- Hastings PJ, Lupski JR, Rosenberg SM, et al. Mechanisms of change in gene copy number. Nat Rev Genet. 2009; 10: 551-564. https://www.nature.com/articles/nrg2593
- Schneider KU, Sabherwal N, Jantz K, et al. Identification of a major recombination hotspot in patients with short stature and SHOX deficiency. Am J Hum Genet. 2005; 77: 89-96. https://www.cell.com/ajhg/fulltext/S0002-9297(07)60904-5
- Newman S, Hermetz KE, Weckselblatt B, et al. Next-generation sequencing of duplication CNVs reveals that most are tandem and some create fusion genes at breakpoints. Am J Hum Genet. 2015; 96: 208-220. https://www.cell.com/ajhg/fulltext/S0002-9297(14)00523-0
Figures:

Figure 1

Figure 2

Figure 3
Similar Articles
-
Partial SHOX duplications associated with various cases of congenital uterovaginal aplasia (MRKH syndrome): A tangible evidence but a puzzling mechanismDaniel Guerrier*,Karine Morcel. Partial SHOX duplications associated with various cases of congenital uterovaginal aplasia (MRKH syndrome): A tangible evidence but a puzzling mechanism. . 2021 doi: 10.29328/journal.jgmgt.1001006; 4: 001-008
Recently Viewed
-
Comparative characterization between autologous serum and platelet lysate under different temperatures and storage timesCamilo Osorio Florez*, Luis Campos, Jessica Guerra, Henrique Carneiro, Leandro Abreu, Andres Ortega, Fabiola Paes, Priscila Fantini, Renata de Pino Albuquerque Maranhão. Comparative characterization between autologous serum and platelet lysate under different temperatures and storage times. Insights Vet Sci. 2023: doi: 10.29328/journal.ivs.1001038; 7: 001-009
-
A Perspective on Conservation Technologies for Endangered Marine BirdsAnn Morrison*, Sonja Lukaszewicz. A Perspective on Conservation Technologies for Endangered Marine Birds. Insights Vet Sci. 2023: doi: 10.29328/journal.ivs.1001039; 7: 010-014
-
Intrauterine Therapy with Platelet-Rich Plasma for Persistent Breeding-Induced Endometritis in Mares: A ReviewThiago Magalhães Resende*,Renata Albuquerque de Pino Maranhão,Ana Luisa Soares de Miranda,Lorenzo GTM Segabinazzi,Priscila Fantini. Intrauterine Therapy with Platelet-Rich Plasma for Persistent Breeding-Induced Endometritis in Mares: A Review. Insights Vet Sci. 2024: doi: 10.29328/journal.ivs.1001045; 8: 039-047
-
Comparing Immunity Elicited by Feedback and Titered Viral Inoculation against PEDV in SwineMaría Elena Trujillo Ortega,Selene Fernández Hernández,Montserrat Elemi García Hernández,Rolando Beltrán Figueroa,Francisco Martínez Castañeda,Claudia Itzel Vergara Zermeño,Sofía Lizeth Alcaráz Estrada,Elein Hernández Trujillo,Rosa Elena Sarmiento Silva*. Comparing Immunity Elicited by Feedback and Titered Viral Inoculation against PEDV in Swine. Insights Vet Sci. 2024: doi: 10.29328/journal.ivs.1001044; 8: 028-038
-
Comparative Analysis of Water Wells and Tap Water: Case Study from Lebanon, Baalbeck RegionChaden Moussa Haidar, Ali Awad, Walaa Diab, Farah Kanj, Hassan Younes, Ali Yaacoub, Marwa Rammal, Alaa Hamze. Comparative Analysis of Water Wells and Tap Water: Case Study from Lebanon, Baalbeck Region. Insights Vet Sci. 2024: doi: 10.29328/journal.ivs.1001043; 8: 018-027
Most Viewed
-
Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization)Dasse Sery Romuald*, KL Siransy, N Koffi, RO Yeboah, EK Nguessan, HA Adou, VP Goran-Kouacou, AU Assi, JY Seri, S Moussa, D Oura, CL Memel, H Koya, E Atoukoula. Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization). Arch Asthma Allergy Immunol. 2024 doi: 10.29328/journal.aaai.1001035; 8: 007-012
-
Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian RandomizationYong-Qing Zhu, Xiao-Yan Meng, Jing-Hua Yang*. Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian Randomization. Arch Asthma Allergy Immunol. 2023 doi: 10.29328/journal.aaai.1001032; 7: 012-022
-
An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergiesNathalie Cottel,Aïcha Dieme,Véronique Orcel,Yannick Chantran,Mélisande Bourgoin-Heck,Jocelyne Just. An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergies. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001027; 5: 030-037
-
Snow white: an allergic girl?Oreste Vittore Brenna*. Snow white: an allergic girl?. Arch Asthma Allergy Immunol. 2022 doi: 10.29328/journal.aaai.1001029; 6: 001-002
-
Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disordersElena Viktorovna Drozdova*. Cytokine intoxication as a model of cell apoptosis and predict of schizophrenia - like affective disorders. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001028; 5: 038-040

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."